Menu
To assess the feasibility of transitioning the management of neglected tropical disease (NTD) campaigns to Ethiopia’s primary health care system, Eyu-Ethiopia, Ethiopia Ministry of Health, and the Collaborative Research and Training Center for NTDs conducted a multi-phase study of the system’s current capacity. This research involved reviewing existing practices for mainstreaming, gathering insights from stakeholders, assessing the system’s preparedness, and engaging stakeholders in developing mainstreaming strategies

Ethiopia is among the countries most impacted by neglected tropical diseases (NTDs). The World Health Organization recently highlighted mainstreaming, which entails transitioning the management of a health campaign from an external organization to the national primary health care system, as beneficial for NTD campaigns. Thus, Ethiopia aims to transition NTD interventions to its primary health care system.
Mainstreaming is context-specific, and its implementation cannot necessarily be generalized from one setting to another. Prior to this study, minimal data were available on the Ethiopia primary health care system’s capacity to handle such a transition
The objectives of this study were to:
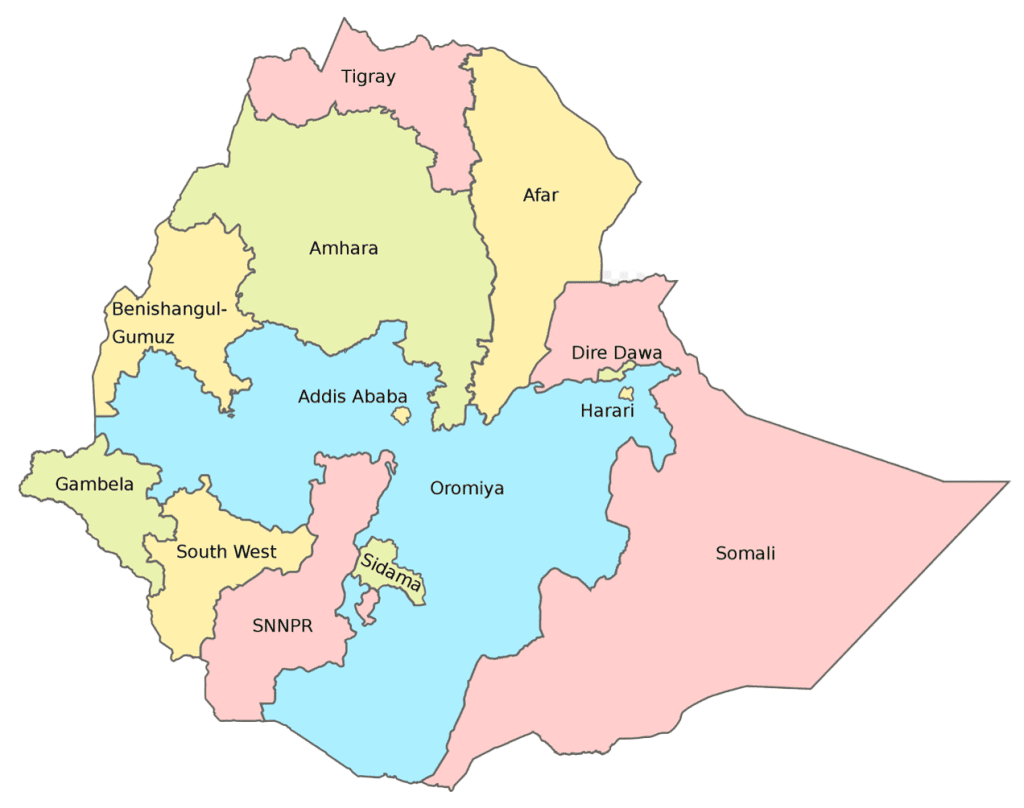
The study locations included eight regions of Ethiopia: Afar, Amhara, Gambela, Oromiya, Sidama, Somalia, SNNPR, and South West.
The findings from this study indicate that currently, Ethiopia’s primary health care system has limited capacity and readiness to fully assume management of NTD interventions. However, partial mainstreaming of NTD campaigns may be feasible.
Through a review of existing mainstreaming practices, researchers found that financing for mainstreamed campaigns is a consistent challenge across various locations. As reflected in the literature, key components for successful mainstreaming include strong governance, community engagement, dedicated funding, and adequate training for health care workers.
Dr. Teshome Gebre of the International Trachoma Initiative walks through the study’s results, lessons learned and promising practices.