Table of Contents
Key Messages
- Health campaigns are time-bound, intermittent activities that address specific epidemiological challenges, expediently fill delivery gaps, or provide surge coverage for health interventions. Campaigns are an important strategy to address high priority diseases (e.g., neglected tropical diseases [NTDs], malaria, polio and other vaccine preventable diseases [VPDs]), and malnutrition (e.g., vitamin A supplementation) across different geographic areas.
- Health campaigns are complex and can be implemented for a short- or long-term need, can be reactive or proactive, and can target a community or subnational/national population. While campaigns have the benefit of targeting specific health needs, multiple campaigns might result in strategic and operational inefficiencies and inequities that can strain health systems, burden health care workers, weaken health services, and limit their long-term health impact.
- Measures of health campaign effectiveness have typically focused on coverage of the intervention’s target population. Yet, there are major data quality and measurement issues around coverage.
- It is important to consider other measures of campaign effectiveness, besides coverage indicators. These indicators should capture both demand-side campaign outcomes (beneficiary acceptability, awareness, and satisfaction) and supply-side campaign outcomes (health worker acceptability, equity, and efficiency). A more encompassing understanding of effectiveness has the potential to improve overall campaign outcomes, enhance population health, and result in stronger, more efficient, and more
equitable health systems.
Purpose
- To provide an introduction to the broad evidence base on the ways that campaigns are defined, the circumstances under which they are used, and the metrics of effectiveness used to reflect the success of campaigns
- To stimulate discussions among country programs, donors, and implementing partners to improve campaign and population health outcomes and to share information across varied programs that use campaigns
Target Audience(s)
- Regional and country-level stakeholders and policy makers who oversee, plan, implement, or monitor health campaigns
- Global organizations that fund, oversee, coordinate, or issue guidance around health campaigns
Introduction
Long-standing public health campaigns have been implemented for neglected tropical diseases (NTDs), malaria, polio and other vaccine preventable diseases (VPDs), and vitamin A supplementation with broad reach around the globe. An integral part of public health strategy, campaigns have been used to provide high coverage of targeted interventions, especially to populations that face challenges in accessing ongoing health services. Health campaigns have also had major impact on disease elimination and eradication efforts. To respond to disease outbreaks, eliminate or eradicate targeted diseases, or achieve other health goals, campaigns and campaign implementation processes have varied across different programs and different geographic settings (1). The most common measure of effectiveness across all health domains is the extent to which a target population is reached with an intervention (i.e., coverage), and supplemented with a focus on the absence of avoidable differences in coverage within the population (i.e., equity). While coverage is an important indicator for the reach of a campaign, other measures of effectiveness are needed to fully understand a campaign’s success and how it is achieved and sustained. For example, the 2016- 2020 strategy for Gavi, the Vaccine Alliance, has four goals for achieving immunization program effectiveness including vaccine coverage, sustainability, health systems, and market shaping (2). These goals are measured using indicators related to coverage, equity, financing, capacity, supply-chain, and community engagement (2). By using such a multi-faceted approach to understanding effectiveness, a broader picture emerges that can show where a campaign’s strengths and weaknesses may fall—allowing for a better understanding of whether campaigns are contributing to equity, efficiency, and health impact.
Methods
We reviewed published and grey literature on campaigns and campaign effectiveness pertaining to neglected tropical diseases (NTDs), malaria, polio and other vaccine-preventable diseases (VPD), and vitamin A supplementation. The focus of our review was on a small sample of references highlighted by experts with extensive experience in conducting campaigns in different countries. The goal was not to conduct a meta-analysis but to identify the most critical information needed to initiate a dialogue on health campaigns and their impact.
Summary of Findings
Campaigns have been an essential strategy for disease prevention, control, elimination, and eradication in addition to ongoing health services for decades. The word ‘campaign’ is commonly used to describe delivery of targeted large-scale health interventions, although this definition varies across public health programs (3,4). Variation also exists in how campaigns report their successes, using a wide range of metrics across and between campaign types. Given this variation, this brief aims to answer the following questions:
- What is a health campaign? What are the key characteristics of health campaigns? What are their strengths and limitations?
- Under what circumstances are health campaigns used to deliver health interventions? What factors influence the decision to deliver an intervention via campaigns?
- What is health campaign effectiveness and how is it measured? What are the measures of campaign effectiveness, and how do they vary across programs and contexts?
What is a health campaign?
According to the International Federation of Red Cross (IFRC), the World Health Organization (WHO), and the United Nations Children’s Fund (UNICEF), the term health campaign is commonly used in reference to “supplementary activities to routine services used to achieve high population coverage” (5). In a systematic review of integration of targeted interventions and health systems, Atun et al found that health campaigns “may be desirable as a temporary measure if the health system (and primary care) is weak; if a rapid response is needed; to gain economies of scale; to address the needs of target groups that are difficult to reach; or to deliver certain very complex services when a highly skilled workforce is needed” (6). Campaigns have been a predominant strategy for delivering health interventions and are planned in a variety of health domains in all WHO regions, but are most heavily relied on in the African region (see Figure 1) (7). While recognizing variation in the goals and delivery methods, the Health Campaign Effectiveness (HCE) Coalition defines campaigns as time-bound, intermittent activities that are deployed to address specific epidemiologic challenges, expediently fill delivery gaps, or provide surge coverage for health interventions (1).

Source: Linksbridge, Campaign Effectiveness and Efficiency
*African Region (AFRO), Region of the Americas (PAHO), South-East Asia Region (SEARO), European Region (EURO), Eastern-Mediterranean Region (EMRO), Western Pacific Region (WPRO) †NTDs include lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminths ‡Vaccines include measles, meningitis, rotavirus, tetanus, typhoid, yellow fever
Characteristics of Health Campaigns
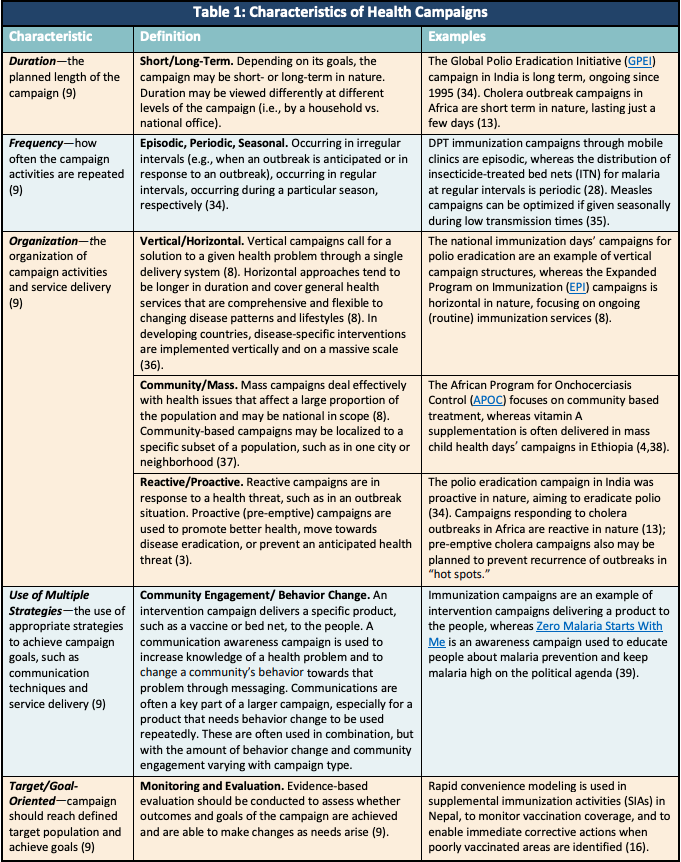
Typically, campaigns are organized in a vertical fashion, which calls for a solution to a given health problem by means of a single delivery system (8). They usually target individuals in a large geographical area (mass population) but can also be focused on a smaller community level.
Campaign design is an important consideration to effectively reach the target population. Depending on the campaigns goal(s) and implementation methods, health campaigns can be categorized based on the following characteristics (9):
- Planned duration of the campaign—short- or long-term in nature. Campaigns may be done in phases or rounds to reach different geographies or to reach the same target population with repeated interventions (10).
- Frequency of activities—occur in regular or irregular intervals depending on seasonality of disease incidence or epidemiological needs (e.g., the development of a sizable group of susceptible individuals)
- Organization of activities and service delivery—depending on these epidemiological needs, campaigns are reactive or pre-emptive in nature. Reactive campaigns respond to a health threat, while pre-emptive campaigns are used to promote better health, move towards disease eradication, and/or prevent an anticipated health threat (3). These factors and coverage goals influence the choice of delivery methods such as door-to-door, fixed point, school-based, transit point, or other methods.
- Use of single or multiple strategies—to achieve campaign goals and reach the target population. When repeated use of a product is desirable, campaigns may rely not only on providing the intervention to the target population but also on fostering a behavior change within that population. These campaigns utilize communications methods, in conjunction with providing a product, to create awareness, increase acceptability, and/or change behaviors.
Strengths and Limitations of Health Campaigns
Strengths
- Credited with delivering health interventions to
millions of people worldwide (1) - Situated to address the needs of specific, hard to-reach populations (11)
- Capable of achieving quick results, and easier to manage than other programs delivered through ongoing health services (8)
- Able to attract political support and funding from donors (8)
- Can be a cost-effective way to achieve high and equitable coverage (12)
Limitations
- Can divert health-care workers from regular duties, causing the temporary halt of ongoing health services (13,14)
- Can result in reallocation of funds and other supplies from ongoing health services. This is due to inadequate financial and human resources that get diverted from the ongoing health system in favor of the campaign (13,14)
- Can result in prioritization of high-profile diseases, regardless of disease burden (15)
- Can show coverage gaps immediately postcampaign, requiring new ongoing distribution channels (12)
Table 1 defines these characteristics in more detail.
Under what circumstances are health campaigns used to deliver health interventions?
Several factors are related to whether a health intervention is delivered a) via a campaign, b) by integrating multiple interventions in campaigns, or c) by integrating campaigns or their components with the primary health care system. *,† These factors, along with examples, include the following:
- Health System Strength (Health System Coverage, Capacity, Equity). Campaigns are often deployed where ongoing health services have insufficient reach or provide coverage to populations that otherwise have insufficient access to care (1).
- Nigeria has the highest frequency of campaigns compared to other countries, and it has a limited universal health care system (1). Similarly, Guinea employs many campaigns, as its primary health care system lacks the infrastructure to respond to outbreaks (11).
- Epidemiology (Disease Control, Emergency Situations, Outbreaks). An area’s epidemiological needs and challenges such as disease control, emergency situation management (e.g., natural or humanitarian disasters), and disease outbreaks should be assessed to determine optimal delivery strategy and campaign timing (1).
- In India, polio has been eradicated; however, polio campaigns continue to supplement ongoing immunization efforts (12). In contrast, cholera campaigns in Africa are primarily introduced during outbreak situations (13). Mass drug administration campaigns for the treatment of lymphatic filariasis are given annually or bi-annually in elimination efforts (14).
- Service Delivery (Access, Availability, Utilization). The geographical demands of health services, poverty numbers and distribution, limited resources (human and financial), and the long-term sustainability of programs will determine the optimal delivery strategy (8,15).
- Measles immunization in Somalia is carried out through campaigns due to poor infrastructure of the health system (1).
- Other National and Global Factors (Political Instability, Global Targets, Donor Priorities). Campaigns must consider the political climate, the type of target they are designed to achieve (e.g., local, national, global), the time frame or urgency of the need, and their ability to accommodate country and donor priorities (1).
- Incentives motivating donors and non-governmental organizations (NGOs) to provide campaign services, such as factors influencing campaign financing, may differ: “the need for quick results to attract political support from their constituents for additional funding in the future or strategic importance of the recipients at that particular moment” (8).
- Population Characteristics (Target Population[s], Demographics, Acceptability). The campaign should be implemented in a way that most effectively reaches the target population. Physical, economic, and socio-psychological aspects of the population must be assessed, as beneficiaries must perceive the care to be accessible and acceptable to them (15). This is where accurate monitoring and evaluation is important, as evidence-based evaluation reveals whether the goals and outcomes of the campaign are achievable (9).
- Rapid convenience modeling is used in supplemental immunization activities in Nepal, to monitor vaccination coverage and enable immediate corrective actions when poorly vaccinated areas are identified (16).
What is health campaign effectiveness and how is it measured?
WHO defines effectiveness as
…the extent to which the programme/initiative’s objectives were achieved or are expected to be achieved, taking into account their relative importance. Effectiveness is also used as an aggregate measure of (or judgement about) the merit of worth of an activity – i.e. the extent to which a programme has achieved, or is expected to achieve, its major relevant objectives and have a positive institutional impact (22).
Metrics to measure effectiveness vary across diseases, strategies, and countries but can be understood at the level of programmatic output (e.g., drug doses delivered), outcome (e.g., campaign coverage), and health impact (e.g., decline in the incidence of disease after the campaign) (1,17). Measures are the broad indicators of program performance, such as coverage or equity; whereas, a metric is a core indicator that quantifies a measure and is comparable between populations (18). Effectiveness measures are centered around programmatic outcomes or health impact:
Programmatic Outcomes
- Coverage—the proportion of the target population receiving the intervention (19)
- Equity—provision of high-quality interventions uniformly and in a fair and impartial manner to all target populations, including underserved groups (19)
- Access—the ease in reaching the health intervention in terms of location, time, and ease of approach (20)
- Efficiency—higher levels of performance (coverage, access, or equity) relative to the inputs (resources, time, money) (19). As an example, cost-effectiveness analysis is the ability to reach populations at the best outcome per dollar spent (1).
- Awareness—increases in awareness, community engagement, and/or change in behavior (21)
Health Impact Indicators
- Disease incidence—changes in the rate of individuals who develop a specific disease or experience a specific health-related event within a period of time (e.g., month or year) (22)
- Morbidity and mortality related to the disease. These may be age-specific rates that relate to a specific time period (2).
The appropriate choice of these measures is determined by the 1) goals of the campaign, 2) available resources for data collection, and 3) political needs (1,23). Table 2 provides examples of the ways that health domains measure campaign effectiveness.
Across health domains, effectiveness is most often measured from the supply side. Coverage is the most frequently used measure of campaign effectiveness. However, utilizing coverage as the sole indicator of campaign effectiveness may not take into account the full complexity of campaign design, and valuable information might be overlooked that would account for contextual elements of a campaign that contribute to, hinder, or are extraneous to success. For example, many campaigns still leave coverage gaps. These gaps may be a result of poor data quality or inadequate monitoring systems due to weak health systems, or may be in relation to another measure of effectiveness not evaluated (1). For example, in 2017 only 31% of mass drug administration campaigns for NTDs reached their coverage targets (24). In studies of insecticide-treated bed net campaigns in Ethiopia, gaps in coverage were associated with both access and behavior change relating to use (25). Meanwhile, many polio campaigns have discordantly reported reaching more than 100% of their target population, demonstrating the difficulty in accurately assessing the numerator and/or the denominator (1). Numerators may be inflated by counting doses administered to persons who were not targeted (e.g., siblings outside of the target age group), and denominators may be either too high or too low because they are often based on outdated data that don’t take into account migration. Additionally, discrepancies may be due to inadequate recording, such as using the count of doses administered without recording which individuals received the intervention (e.g., using tally sheets to count doses delivered versus using home-based records) (26). These data quality issues can divert resources and draw attention away from disease programs, such as happened in Burkina Faso where a large measles outbreak occurred in 2009 despite vaccination coverage reported at greater than 95% (27). Data on coverage are often nationally aggregated, which limits a country’s ability to accurately monitor progress (28). This may mask subnational differences in campaign performance.
While coverage is the measure commonly used across all health domains, gaps that are not addressed by coverage indicators may be better understood through other measures of effectiveness. These include those related to the supply side such as equity, efficiency, and health worker acceptability, and to the demand side in terms of beneficiary acceptability, accessibility, awareness, and satisfaction. Measures to consider may include the perceived quality of the care provided, as well as other social determinants contributing to the access of an intervention including affordability, accessibility, and availability. These measures are important for determining systemic issues that hinder service delivery and thus contribute to lower coverage and equity (29). Additional measures that may be important for understanding the extent to which a campaign is or is not reaching coverage targets include awareness and acceptability, especially for campaigns that rely on a high level of behavior change or community engagement. This is influenced in part by perceived need by the target population, as individuals who do not think an intervention is needed are unlikely to partake in it, even if it is free (29). Community health workers may address some of these gaps by increasing the intervention’s acceptability by and access to the population, though more research is needed to determine if this is true in all campaign contexts (30). While the aforementioned issues are important to consider, this is not an exhaustive list of measures to be explored.
The complexity and context of a health campaign should be considered when selecting measures of effectiveness (31). To best understand what aspects of a campaign directly impact the outcomes, campaigns must identify “which elements belong to the intervention (and therefore participate in its effects and can be transferred), which ones belong to the context and interact with the former to influence results (and therefore must be taken into account when transferring the intervention) and which contextual elements are irrelevant to the intervention” (32). Because weak health systems often have inadequate monitoring systems leading to difficulties collecting reliable data, effectiveness measures for health interventions often lack comprehensive metrics (31).
Conclusions
A common understanding and use of metrics for campaign effectiveness will aid in determining campaign success in a variety of contexts. Given the complexity of campaigns, without more robust use of effectiveness metrics important and valuable data may not be collected. This creates gaps in the ability to identify factors determining whether a campaigns target goals are met.
A shared understanding of the combination of metrics and measures to best determine campaign effectiveness is important to
- Build a knowledge base of what works and generate a process of shared learning among campaigns;
- Improve the quality of decision making;
- Foster interdisciplinary dialogue among stakeholders of campaigns; and
- Sustain interest in, and funding for, health campaigns that demonstrate positive outcomes (17).
Currently, the majority of campaigns focus on quantitative measures of effectiveness, specifically in terms of coverage, and give minimal consideration to qualitative measures, such as those that contribute to acceptability. By broadening the evidence base of metrics to determine campaign effectiveness, data compiled through cross-campaign sharing may allow for improvement in identifying and correcting shortfalls in reaching target goals. This will in turn lead to a better understanding of “whether the objectives formulated in the programme are being achieved, what the successes and difficulties have been, how appropriate the solutions chosen have been and what the influence is of factors external to the programme” (33).
Fostering discussion among campaign planners to determine the appropriateness of metrics can lead to improved understanding of campaign performance, effectiveness, and efficiency through shared learning. Addressing the evidence gaps relating to campaign effectiveness metrics will help to promote transparency and accountability of public health campaigns (17).
Evidence Gaps
The following issues contribute to evidence gaps related to defining a health campaign and campaign effectiveness:
- Poor data quality impacts the reliability of using coverage as a sole indicator of effectiveness. Coverage is measured in a variety of ways, but gaps show that there are some issues in data quality that disallow accurate cross-campaign comparison. This may be in part due to nationally aggregated data masking subnational disparities in effectiveness.
- Other measures are needed to comprehensively explore effectiveness. Coverage measures are the most prevalent ones used for campaign effectiveness, but coverage is only one component. Other measures of health and programmatic outcomes need to be identified and used so campaigns can choose a more comprehensive approach to identify the components that make them more effective in achieving target outcomes.
- Efforts should be undertaken to determine measures needed for different campaigns given their contexts. Developing guidance on when it is appropriate to choose a specific measure for a given campaign.
- Metrics are needed for determining equity, efficiency, accessibility and acceptability. All are important components of campaigns, but metrics are lacking for many domains in how to best evaluate these.
Future Opportunities
Discussions among stakeholders and implementation research is needed for the development of guidelines or frameworks to enable programs to choose the most appropriate measure(s) and metric(s) to assess campaign effectiveness in different contexts. The findings will contribute to building a shared understanding of different measures of campaign effectiveness. This shared learning will facilitate the understanding of factors that lead to successes and failures of campaigns in reaching their coverage goals.
Acknowledgements
We would like to acknowledge the following experts who provided valuable inputs in the process of developing this brief:
Task Force for Global Health
Alan Hinman
Kristin Saarlas
Carol Tangum
Katherine Gass
UNICEF
Andreas Hasman
Linksbridge
Heather Ferguson
KJ Zunigha
Julia Mulroy
Contact
For more information on this topic or to discuss further with the Health Campaign Effectiveness team, please visit www.campaigneffectiveness.org or contact the program directly at: campaigneffectiveness@taskforce.org.

References
- Camber Collective. The Campaign Effectiveness Landscape and Case for Action (2020). Developed by Camber Collective in partnership with the Bill & Melinda Gates Foundation and the Task Force for Global Health. Available from https://campaigneffectiveness.org/resources/landscape-and-case-for-action/
- Gavi, The Vaccine Alliance. Gavi strategy phase 4 (2016-2020). 2014. Available from: https://www.gavi.org/our-alliance/strategy/phase-4-2016-2020
- Mbabazi WB, Tabu CW, Chemirmir C, Kisia J, Ali N, Corkum MG, et al. Innovations in communication technologies for measles supplemental immunization activities: lessons from Kenya measles vaccination campaign, November 2012. Health Policy Plan 2015;30(5):638–44.
- Gatobu S, Horton S, Kiflie Aleyamehu Y, Abraham G, Birhanu N, Greig A. Delivering vitamin A supplements to children aged 6 to 59 months: comparing delivery through mass campaign and through routine health services in Ethiopia. Food Nutr Bull 2017;38(4):564–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28528554
- IFRC, WHO, UNICEF. Community-based health care, including outreach and campaigns, in the context of the COVID-19 pandemic. Interim guidance, May 2020. Available from: https://www.who.int/publications-detail/community-based-health-care-including-outreach-and-campaigns-in-the-context-of-the-covid-19-pandemic
- Atun R, de Jongh T, Secci F V, Ohiri K, Adeyi O. Clearing the global health fog: a systematic review of the evidence on integration of health systems and targeted interventions. Washington DC: The World Bank, 2009. Available from https://documents.worldbank.org/en/publication/documents-reports/documentdetail/645941468341113496/clearing-the-global-health-fog-a-systematic-review-of-the-evidence-on-integration-of-health-systems-and-targeted-interventions
- Global Campaigns Overview. Campaign effectiveness and efficiency [Internet]. [cited 2020 Aug 24]. Available from: https://campaign-effectiveness.squarespace.com/global-campaigns-overview
- Msuya J. Horizontal and vertical delivery of health services: what are the trade offs? Part of a background study on Making Services Work for Poor People prepared for the World Development Report), 2003. Available from: http://documents1.worldbank.org/curated/en/914491468761944686/310436360_200502761000211/additional/269420Msuya1WDR1Background1paper.pdf
- Watson C, James R. What is a health promotion campaign? What then constitutes a campaign? What makes it different from a program? Characteristics of a health promotion campaign. Health Promot J Aust 1991;1(1):3–5.
- Galatas B, Saúte F, Martí-Soler H, Guinovart C, Nhamussua L, Simone W, et al. A multiphase program for malaria elimination in southern Mozambique (the Magude project): a before-after study. PLOS Medicine 17(8):e1003227. https://doi.org/10.1371/journal.pmed.1003227
- Shoman H, Karafillakis E, Rawaf S. The link between the West African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: a systematic review. Global Health 2017;13(1):1.
- Chakrabarti A, Grépin KA, Helleringer S. The impact of supplementary immunization activities on routine vaccination coverage: an instrumental variable analysis in five low-income countries. PLOS One 14(2): e0212049. Available from: https://doi.org/10.1371/journal.pone.0212049
- Teshome S, Desai S, Kim JH, Belay D, Mogasale V. Feasibility and costs of a targeted cholera vaccination campaign in Ethiopia. Hum Vaccines Immunother 2018;14(10):2427–33. Available from: https://doi.org/10.1080/21645515.2018.1460295
- WHO. Assessing the epidemiology of soil-transmitted helminths during a transmission assessment survey in the global programme for the elimination of lymphatic filariasis. 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/153240/9789241508384_eng.pdf?sequence=1
- Health Service Delivery [Internet]. 2010 [cited 2020 Aug 17]. Available from: https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_section1_web.pdf?ua=1
- Oh DH, Dabbagh A, Goodson JL, Strebel PM, Thapa S, Giri JN, et al. Real-time monitoring of vaccination campaign performance using mobile phones—Nepal, 2016. MMWR Morb Mortal Wkly Rep 2016;65(39):1072–6.
- Murray CJL, Frenk J. Health metrics and evaluation: strengthening the science. Lancet 2008;371:1191-99.
- Health System Metrics. Report of a technical meeting, Glion, Switzerland, 28-29 September 2006. Draft report, 2006. Available from: https://www.who.int/healthinfo/health_system_metrics_glion_report.pdf
- Health Campaign Effectiveness Coalition. Glossary. [Internet]. [cited 2020 Aug 24]. Available from: https://campaigneffectiveness.org/glossary/
- WHO. Health Systems Strengthening Glossary [Internet]. [cited 2020 Aug 11]. Available from: https://www.who.int/healthsystems/hss_glossary/en/
- Seymour J. The impact of public health awareness campaigns on the awareness and quality of palliative care. J Palliat Med 2018;21(S1):S30-S36. doi: 10.1089/jpm.2017.0391.
- Obesity Prevention Source. Prevalence and incidence defined. Harvard T.H. Chan School of Public Health [Internet]. [cited 2020 Aug 18]. Available from: https://www.hsph.harvard.edu/obesity-prevention-source/prevalence-incidence/
- Mills A. Mass campaigns versus general health services: what have we learnt in 40 years about vertical versus horizontal approaches? Bull World Health Organ. 2005;83(4). Available from: https://apps.who.int/iris/bitstream/handle/10665/73185/bulletin_2005_83%284%29_315-316.pdf?sequence=1&isAllowed=y
- Bill and Melinda Gates Foundation. Global Grand Challenges. Innovations for improving the impact of health campaigns (Round 24). [cited 2020 Aug 11]. Available from: https://gcgh.grandchallenges.org/challenge/innovations-improving-impact-health-campaigns-round-24
- Birhanu Z, Abebe L, Sudhakar M, Dissanayake G, Yihdego Y, Alemayehu G, et al. Access to and use gaps of insecticide-treated nets among communities in Jimma Zone, southwestern Ethiopia: baseline results from malaria education interventions Infectious Disease epidemiology. BMC Public Health 2015;15(1):1–11.
- WHO. Practical guide for the design, use, and promotion of immunization of home-based records in immunization programmes. 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/175905/WHO_IVB_15.05_eng.pdf?sequence=2
- Edelstein M. Measuring vaccination coverage better will help achieve disease control. Intl Health 2017;9(3):142–4. https://doi.org/10.1093/inthealth/ihx013
- WHO. Primary health care on the road to universal health coverage, 2019 global monitoring report. Available from: https://www.who.int/healthinfo/universal_health_coverage/report/uhc_report_2019.pdf?ua=1
- Shengelia B, Tandon A, Adams OB, Murray CJ. Access, utilization, quality, and effective coverage: an integrated conceptual framework and measurement strategy. Soc Sci Med;2005;61(1):97–109.
- Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs 2002;19:11–20. doi: 10.1046/j.1525-1446.2002.19003.x
- Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health 2002;56(2):119-27. doi: 10.1136/jech.56.2.119.
- Minary L, Alla F, Cambon L, Kivits J, Potvin L. Addressing complexity in population health intervention research: the context/intervention interface. J Epidemiol Community Health 2018;72(4):319–23.
- WHO. WHO evaluation practice handbook. 2013. Available from: https://apps.who.int/iris/handle/10665/96311
- Thacker N, Vashishtha VM, Thacker D. Polio eradication in India: the lessons learned. Pediatrics 2016;138(4):e20160461; DOI: https://doi.org/10.1542/peds.2016-0461.
- Thakkar N, Gilani SSA, Hasan Q, McCarthy KA. Decreasing measles burden by optimizing campaign timing. Proc Natl Acad Sci USA 2019;166(22):11069–73.
- Orenstein WA, Seib K. Beyond vertical and horizontal programs: a diagonal approach to building national immunization programs through measles elimination. Expert Rev Vaccines 2016;15(7):791–3.
- Deardorff KV, Rubin MS, Ásbjörnsdóttir KH, Walson J. Strategies to improve treatment coverage in community-based public health programs: A systematic review of the literature. PLoS Negl Trop Dis 2018 Available from: https://doi.org/10.1371/journal.pntd.0006211
- WHO. African Programme for Onchocerciasis Control. Available from: www.who.int/apoc
- WHO. World Malaria Day 2020. Available from: https://www.who.int/campaigns/world-malaria-day/world-malaria-day-2020.
- USAID. Neglected Tropical Disease Program, Results. Available from: https://www.neglecteddiseases.gov/about/results.
- WHO. Achieving and maintaining universal coverage with long-lasting insecticidal nets for malaria control. 2017. Available from: https://www.who.int/malaria/publications/atoz/who_recommendation_coverage_llin/en/
- WHO. Indicators to measure the impact of malaria control (archived). 2000. Available from: https://www.who.int/malaria/publications/atoz/whocdsrbm200022/en/
- The Alliance for Malaria Prevention. AMP toolkit. 2018. Available from: https://allianceformalariaprevention.com/amp-tools/amp-toolkit/
- Global Polio Eradication Initiative. GPEI tools, protocols and guidelines. Available from: http://polioeradication.org/tools-and-library/resources-for-polio-eradicators/gpei-tools-protocols-and-guidelines/
- Global Vaccine Action Plan, 2011-2020. Annex 6: the monitoring and evaluation/accountability framework. WHO, 2013. Available from: https://www.who.int/docs/default-source/vaccines-and-immunization/gvap-annex6.pdf?sfvrsn=c1b69971_2
- UNICEF. Vitamin A supplementation: a decade of progress [Internet]. 2007 [cited 2020 Apr 23]. Available from: https://www.unicef.org/publications/files/Vitamin_A_Supplementation.pdf
